Cholera in 19th-century Singapore
The colony experienced its first cholera outbreak in 1841, and several epidemics in the decades thereafter. Bonny Tan examines how the battle against this deadly illness was won.
 View of Boat Quay looking towards Fort Canning Hill, 1890s. As the centre for trade and commercial activity in Singapore in the 19th century, the Singapore River became highly congested and polluted, resulting in poor drainage and unsanitary living conditions along the river banks. The river water was blamed for causing various diarrhoea-inducing diseases, including cholera. Andrew Tan Collection, courtesy of National Archives of Singapore.
View of Boat Quay looking towards Fort Canning Hill, 1890s. As the centre for trade and commercial activity in Singapore in the 19th century, the Singapore River became highly congested and polluted, resulting in poor drainage and unsanitary living conditions along the river banks. The river water was blamed for causing various diarrhoea-inducing diseases, including cholera. Andrew Tan Collection, courtesy of National Archives of Singapore.
At the beginning of the 19th century, a mysterious disease circled the globe, eventually killing millions in its wake. Although the cause was unknown, its outcome was severe; within hours of vomiting and diarrhoea, a healthy person would be sickened, along with those who had been in close contact with the infected.
Endemic to India’s Ganges Basin, the first recorded pandemic of this ailment called cholera began in 1817. Before long, it spread like wildfire throughout Asia, giving it the nickname – the Asiatic Cholera. Riding on the backs of colonialism and the increased trade ties that spanned the oceans, the pestilence travelled beyond Asia to Europe and the Americas. To date, the world has experienced at least seven known cholera pandemics.
Singapore, with its strategic location along major trade routes, was not spared. When the scourge afflicted the island in the 1840s, the British colonial authorities responded by improving the settlement’s healthcare, waterworks and sanitation. Although occurring more than a century ago – the unending waves of cholera, the subsequent cures and medicines, and the unfolding of scientific understanding and control of the disease, has resonance with the Covid-19 pandemic that Singapore is experiencing today.
The First Outbreaks in Singapore
The disease first reached the Malay Peninsula with “explosive suddenness” in Penang in October 1819, just nine months after the founding of Singapore. Anticipating its spread southwards, cholera medication was quickly dispatched to the colony and the new settlement was spared.
The next two decades were uneventful until Singapore’s first cholera outbreak in April 1841, affecting especially the “Native and Portuguese” people living in Telok Ayer.1 The disease was probably introduced to the island through the Anglo-Indian trade routes as well as British troops travelling en route to China to fight in the First Opium War (1839–42). Thereafter, cholera took firm root in Singapore, rearing its ugly head periodically.
At the time, Singapore was ill-equipped to handle the cholera outbreak because of a lack of proper medical care and insufficient hospital beds. As a result, in May 1841, the cholera-stricken seamen on the battleship H.M.S. Pelorus were not allowed to disembark on the island. Responding to the situation, the colonial government set up the European Seamen’s Hospital in November 1842,2 a predecessor of the Singapore General Hospital.
In 1851, Singapore faced its second cholera outbreak. This time around, the impact on the community was so severe that it quickly escalated into an epidemic. Lasting between January and May 1851, the epidemic gravely affected the population in Kampong Glam. By 25 April, an estimated 220 people had died, of whom 107 were Malays and 95 Chinese, although some reports suggest that the death toll reached as high as 400 at one point.3 The severity of this epidemic led to calls for proper waterworks and drainage to clear sewage among the coolie community quarters where the largest number of deaths occurred.
Although there were no other major outbreaks in Singapore in the 1860s, an epidemic that took place in Mecca in 1865 was traced to the colony. That episode killed 15,000 out of the approximately 90,000 pilgrims in Mecca and was linked to British ships originating from Singapore with Javanese pilgrims on their way to the haj.4
Singapore’s next cholera epidemic occurred in 1873, this time crossing over from Bangkok via the S.S. Chow Phya on 2 July. In just three months, 448 of the 857 known cases died, chalking up an alarming mortality rate of over 50 percent.5 This led to stricter quarantine laws and sanitary measures, which helped to stem the spread of the disease.
Despite these actions, cholera returned to Singapore with a vengeance two decades later, beginning with a sudden surge of deaths among Chinese coolies in April 1895 compared to the same period the prior year. This was the first indication that something sinister was afoot, but before any action could be taken by the authorities, there was a sudden spike in cholera cases between June and August that year. Subsequently, calls were made for a more systematic count of deaths and their causes so that future outbreaks could be nipped in the bud.6
Understanding Cholera
Cholera is caused by the bacterium Vibrio cholerae, which was identified by German scientist Robert Koch in 1883. The bacterium enters the body when contaminated food or water is ingested. In the small intestine, the bacterium reproduces in the mucous lining of the bowels. While most victims are asymptomatic or display limited symptoms, at least 20 percent are severely affected.
As the immune system of the infected person attempts to fight the bacteria, a poison released by the bacteria causes the intestinal walls to work in reverse: instead of food nutrients moving into the bloodstream, plasma from the blood drains into the intestines, causing the distinctive “rice water stools” associated with this illness.7 Copious amounts of this liquid are then expelled by the sick person resulting in dehydration. If untreated, it can lead to shock and eventually death.
In the 19th century, the scientific study of germs was still in its infancy. The prevailing belief was that the malady was spread through effusions of bad air released by rotting material. Based on this miasmic theory of the disease, people in the Western world were encouraged to keep away from foul air during cholera outbreaks. Posters like the “Cholera Prevention Man”, distributed throughout Europe and America, depict a man surrounded by a cabinet of potions and covered in layers of clothing to protect himself from the “bad air”, and inhaling as an antidote the clean air of vinegared vapours released from a bottle.
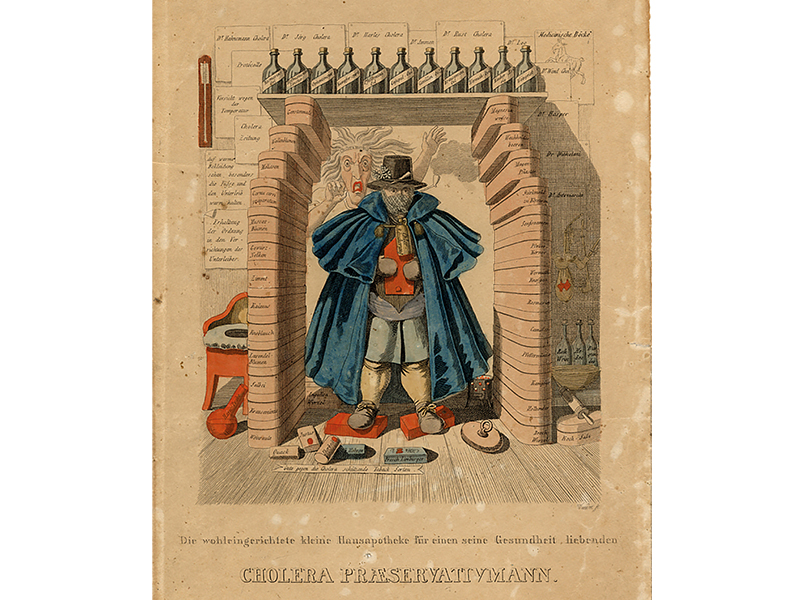 An ink and watercolour etching of the “Cholera Prevention Man” by Wundet. The translation of the inscription reads: “The well-equipped home medicine cabinet for one who loves his health. Cholera Prevention Man”. Division of Medicine and Science, National Museum of American History, Smithsonian Institution.
An ink and watercolour etching of the “Cholera Prevention Man” by Wundet. The translation of the inscription reads: “The well-equipped home medicine cabinet for one who loves his health. Cholera Prevention Man”. Division of Medicine and Science, National Museum of American History, Smithsonian Institution.
Certainly, there was no shortage of “bad air” in the slums of 19th-century Singapore as new migrants arrived by the shipload, with many squeezed into congested and unhygienic quarters along the stretch of the Singapore and Kallang rivers. There, poor drainage and improper disposal of sewage, along with the foul detritus of activities like pig-breeding resulted in “the first-class stenches that Singapore slums so successfully distil”.8 The Singapore River at low tide was compared to the River Thames in London, revealing the filth that caused the foul air seen as the root of various diseases, including cholera.
Contaminated water was later proven to be a conduit for the disease, especially given the poor hygiene practices in the consumption of food and drink among local residents. Raw fruit and vegetables were one source of infection, as were the shellfish plucked from the murky Singapore River. Popular among the Chinese community, the shellfish was described as “dainties which thrive on sewage and afford a breeding ground for microbes”. The situation was further aggravated by the consumption of contaminated well water as well as water bottled from the polluted Kallang River.9
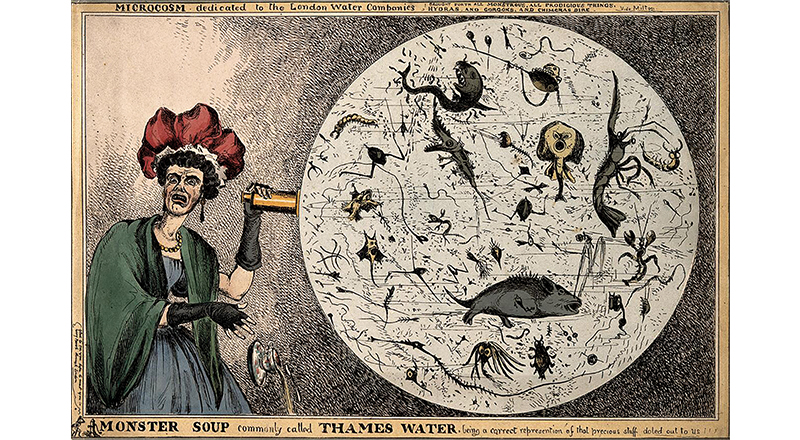 A cartoon showing a woman dropping her teacup in horror upon discovering the monstrous contents of a magnified drop of water from the River Thames, revealing the impurity of drinking water in London. Coloured etching by William Heath, 1828. Wellcome Collection. Attrbution Non-commercial (CC BY-NC 4.0).
A cartoon showing a woman dropping her teacup in horror upon discovering the monstrous contents of a magnified drop of water from the River Thames, revealing the impurity of drinking water in London. Coloured etching by William Heath, 1828. Wellcome Collection. Attrbution Non-commercial (CC BY-NC 4.0).
Following the tragic outcomes of the 1851 epidemic, a decision was made to set up proper waterworks in Singapore. In 1852, the Government Surveyor John Turnbull Thomson drew up plans for supplying water to the town, although it was only in 1867 that the Impounding Reservoir (later renamed MacRitchie Reservoir) was approved for construction off Thomson Road. The reservoir finally began operations in 1877.10
Local Cures and Customs
Globally, there was no agreed method for treating cholera in the 19th century. In the early days of the epidemics, residents in Singapore turned to remedies that had been adopted in countries where pandemics had previously swept through.
One recipe recommended by a Major Wallace of the Madras Presidency in British India involved imbibing brandy infused with cloves, cinnamon and peppers, and topped with laudanum, an opiate. The cure was first published in The Asiatic Journal and Monthly Register for British and Foreign India, China and Australasia in July 1838, and reprinted in The Singapore Free Press on 1 April 1841. The remedy was touted as a success in India and Germany.
Unfortunately, the same outcomes were not realised in Singapore when the Straits Settlements Medical Officer Thomas Oxley administered this potion to five patients here. In a critical letter to The Singapore Free Press on 15 April 1841, he recommended the use of “hot salt water emetics and enemata, aided by dry heat to the surface of the body” instead as a cure.11
Other treatments put forward at the time included a concoction by Queen Victoria’s physician James Clerk “which proved very effectual in England in 1849”, mixing equal parts of camphor, laudanum, turpentine and peppermint. Another prescription attributed to a Lord Ponsonby comprised dissolving “one part camphor in six parts of spirits of wine”.12 People in Singapore had their own home remedies. In 1849, one Charles Perreau found his cure in a traditional Malay approach consisting of bruised ginger boiled in a pint of water for 10 minutes, with two tablespoons of salt added. This was consumed while the body was briskly rubbed.
In a letter to The Singapore Free Press in October 1849, Perreau wrote: “After having tried every European remedy I received no benefit, and were it not for a simple Malay Drug I would not have recovered from my severe attack nor would I, Mr Editor, now have been able to address you upon the subject.”13 It may have been a “simple Malay Drug” but this remedy is not dissimilar to the World Health Organization’s modern-day recommendation to drink clean water mixed with sodium and glucose to replace the loss of salts and liquids, and prevent dehydration.
Singapore’s Asian residents were often reluctant to seek treatment in government hospitals out of fear and superstition, preferring native remedies instead. For this reason, police stations and kongsi (clan) houses were stocked with a local concoction for treating cholera well into the early 20th century. This pungent mix of calumba, cardamon, ammonia, camphor and capsicum, steeped in peppermint water, was first offered during the 1851 outbreak in Singapore and was considered a trustworthy curative.14
In the late 19th century, the Chinese also turned to their own dispensaries along Philip Street, imbibing “Chinese red pills” and a trusty homemade remedy of old ginger infused in hot water. On their preference for Asiatic medicines, one Peranakan gentleman wrote: “Cholera is an Asiatic disease, it is within the province of the Asiatic people and their physicians to know something about the disease…”15
Native cures went beyond mere medication. During outbreaks, loud communal processions to exorcise the “Hantu Cholera”,16 or cholera demon, took place nightly. The Chinese would parade around town “escorting fierce gladiators carried on platforms with drawn swords and flags with which they cut the air in all directions while the demon was roused up with the din of gongs and cymbals. As these processions pass, their countrymen rush out and let off crackers to their own intense gratification and the great annoyance of hack and private carriage drivers”.17
There were also Indian processions, which were described as a “little less dangerous, accompanied as they are by the ringing of bells, blowing of horns, and clamorous beating of tom toms”. The Malays added to the general din by “bawling out in the streets at a late hour of the night, rendering sleep next to impossible to the great bulk of the town residents”.18
In 1873, the Colonial Secretary James Birch participated in a Tamil procession and was garlanded in appreciation for his support. This created some controversy at the Legislative Council when Dr Robert Little, a medical practitioner who also served as a council member, argued that such processions where “persons went about with knives and swords, crying out, and howling and screaming… fighting with fancied deities and spirits” not only caused unrest and obstructions, but also amplified fear among local residents and “were the cause of spreading cholera instead of preventing it”.19
Nevertheless, some local approaches to the disease had their advantages. For example, during the 1851 cholera epidemic, medical authorities used native drums to inform the locals whenever hospital palanquins made their rounds so that the sick could be quickly conveyed to hospital.20
Quarantine Quarrels
The first recorded instance of forced quarantine in Singapore took place in June 1821 when the cholera-stricken Austrian ship, the Caroline Augustus, arrived from Batavia (now Jakarta) with afflicted sailors. Mindful of the safety of residents in Singapore who were “relatively untouched by cholera”, the colonial authorities did not permit the ship to land except to have their convalescents disembark at Sandy Point21 (on the tip of Tanjong Rhu today) where medical assistance was rendered.
However, strict quarantine measures were not consistently applied to the growing number of ships arriving in Singapore until the severity of the 1851 cholera epidemic, followed by a smallpox outbreak in 1857, called for a re-evaluation. One of the recommendations made to Governor of the Straits Settlements Edmund A. Blundell was that every vessel be checked for illness and that an infected ship be quarantined, with no one permitted to leave until every person on board was given a clean bill of health. Only those bringing medical or food supplies to the ship would be allowed to board.22
Governor Blundell, however, noted that no vessels could be completely free of contagious diseases and that such actions would interfere with the “free immigration” and “agricultural interests” that the Straits Settlements offered.23 Quarantine was also seen as an annoyance by the mercantile community as it hindered the free flow of trade. To complicate matters, not everyone in the medical field was convinced that quarantine was an effective means of keeping diseases out of Singapore.
In 1866, the British Cholera Commission, having had the experience of battling severe cholera outbreaks in England, advised the British Governor-General of India that cholera was a communicable disease and reccommended that infected persons be quarantined to stem the contagion. In the Straits Settlements, new ordinances for quarantine were soon introduced.
However, Dr Little, who had by then served 28 years in Singapore, strongly opposed the quarantine bill in 1868. He noted that residents in Singapore had acquired immunity as cholera had been endemic here for more than 20 years, adding that quarantine would affect the entrepot trade that Singapore had become so reliant on. The setting up of a lazaretto (a facility to isolate and treat people with contagious diseases) would also incur too high a cost. Nevertheless, in November 1868, Governor Harry St George Ord issued the order for the quarantine bill.24
The bill would lead to the proposal to set up a lazaretto on St John’s Island. Following the cholera epidemic that was introduced to Singapore by a ship from Bangkok in 1873, Acting Master Attendant Henry Ellis proposed a scheme which “included a steam cutter, a floating police station, a hospital on St John’s, and a quarantine burial-ground on Peak [Kusu] Island”.25 The lazaretto was seen as an ideal solution as infected patients could be sent to St John’s Island to recover while the ships they disembarked from could continue on their journey unhindered.
In November 1874, the S.S. Milton arrived from Swatow (now Shantou), China, with around 1,200 to 1,300 Chinese coolies on board. It was suggested that at least two of them had died of cholera upon arrival, although contaminated water purchased in Singapore could also have been a source of infection.26
As the lazaretto on St John’s Island had not been completed yet, huts had to be quickly constructed at personal cost to the ship’s agents to accommodate the sick. The lazaretto was eventually completed in 1875.27 St John’s would be used as a quarantine centre for the next hundred years until its facilities were officially closed in January 1976.28
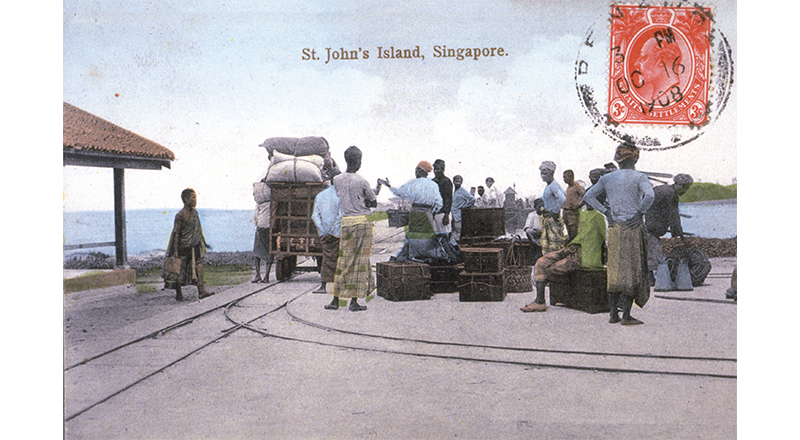 Newly arrived migrants at the quarantine centre on St John’s Island, waiting for the ferry to take them to mainland Singapore, c. 1908. Courtesy of National Archives of Singapore.
Newly arrived migrants at the quarantine centre on St John’s Island, waiting for the ferry to take them to mainland Singapore, c. 1908. Courtesy of National Archives of Singapore.
Putrid Pitholes
As late as 1889, Singapore had yet to have a proper sewage system in place, aggravating the situation whenever cholera outbreaks took place.29 According to the Acting Health Officer Dr Gilmore Ellis, four-fifths of toilets here had “no catchment apparatus whatever other than the bare earth (with or without a hole dug in it) or a large cesspool built of brick… [which] retain larger accumulations of excrement… that not unfrequently is one mass of writhing maggots to be removed…”30
The bucket system in use at the time involved the manual removal of faeces, or night soil, carried to places outside of town and disposed of by coolies. While it was an improvement over foul-smelling cesspits located near residences, the bucket system had its own share of problems. The system relied on lowly paid and poorly motivated night-soil workers to clear the buckets regularly. In addition, the subsequent disposal of the waste and the washing of the night-soil buckets had to be done in such a way that groundwater and rivers did not become contaminated.
 A night-soil carrier, c. 1940. Workers were paid to manually remove human waste. The workers would arrive at households with empty buckets to exchange for filled ones. As the collection was usually carried out at night and the filled buckets covered with soil to lessen the stench, it soon acquired the name “night soil”. Courtesy of National Archives of Singapore.
A night-soil carrier, c. 1940. Workers were paid to manually remove human waste. The workers would arrive at households with empty buckets to exchange for filled ones. As the collection was usually carried out at night and the filled buckets covered with soil to lessen the stench, it soon acquired the name “night soil”. Courtesy of National Archives of Singapore.
The 1895 cholera epidemic renewed discussions over how the disposal of night soil could be improved. There was a call for the authorities to organise a proper network of night-soil carriers to do the job, while the Health Officer pushed for the reconstruction of unsanitary toilets and ordered public latrines to be cleaned regularly with Jeyes Fluid, a disinfectant still used today.31
| MOULE’S ECO-TOILET |
| The world’s “first practical earth-closet”, a composting toilet for homes without access to piped water has an indirect connection to Singapore. It was invented in England by Reverend Henry Moule, the brother of Reverend Horatio Moule, Resident Chaplain at Singapore’s St Andrew’s Chapel between 1845 and 1851. |
| Seeing how cholera outbreaks in England in the mid-19th century were caused by poor sanitation, Henry Moule designed a dry-earth toilet as a hygenic means of disposing human waste. He patented his earth-closet in 1860 and is acknowleged today as its inventor. |
| The earth-closet resembled a modern-day toilet, with a hole cut into a chair, a bucket below it and a hopper filled with earth attached to the back of the seat. When a handle was pulled, a quantity of earth would be released over the human excreta to mask unwelcome odours and help the contents to decompose. When the bucket was full, the resulting compost could be used to enrich and fertilise soil. Moule was certainly ahead of his time when he came up with this contraption. |
 Reverend Henry Moule – the brother of Reverend Horatio Moule, Resident Chaplain at the St Andrew’s Chapel in Singapore – invented the “first practical earth-closet”. Henry Moule patented his design in 1860. Seen here is the improved version of Moule’s environment-friendly toilet, c. 1875.Retrieved from Wikimedia Commons (CC BY-SA 3.0). Reverend Henry Moule – the brother of Reverend Horatio Moule, Resident Chaplain at the St Andrew’s Chapel in Singapore – invented the “first practical earth-closet”. Henry Moule patented his design in 1860. Seen here is the improved version of Moule’s environment-friendly toilet, c. 1875.Retrieved from Wikimedia Commons (CC BY-SA 3.0). |
| REFERENCES |
| BBC. (2014). Moule’s mechanical dry earth closet. Retrieved from BBC website. |
| Earth closets. (n.d.). Retrieved from Old & Interesting website. |
| Russell, M. (2014, February). Life of Reverend Henry Moule M.A. (1801–1880). Retrieved from RootsWeb website. |
| Sipe, B.M. (1988). Earth closets and the dry earth system of sanitation in Victorian America. Material Culture, 20 (2/3), 27–37. Retrieved from JSTOR via NLB’s eResources website. |
Finally, a Vaccine
Singapore would experience its most severe cholera outbreak in 1902 when 759 out of the reported 842 cases died, a hitherto unprecedented mortality rate of 90 percent.32 This, however, was the last time that cholera would exact such a heavy toll here as modern developments in sanitation and waterworks helped control the spread of the disease.
Advancements in medical science in subsequent years also brought a greater understanding of the disease, identifying its cause and controlling it through the development of a vaccine. Following Koch’s identification of Vibrio cholorae in 1883, Spanish doctor Jaime Ferran, who trained under the famed microbiologust and chemist Louis Pasteur, successfully immunised humans against cholera in 1885.33 By the 1920s, Singapore was receiving a supply of vaccines from the Pasteur Institute in Bandung, Java.34 In the 1930s, the Institute of Medical Research in Kuala Lumpur began producing supplies of the cholera vaccine not only for Malaya but for the region too.35
 A child being vaccinated against cholera at one of several inoculation centres in Singapore, 1963. Ministry of Information and the Arts Collection, courtesy of National Archives of Singapore.
A child being vaccinated against cholera at one of several inoculation centres in Singapore, 1963. Ministry of Information and the Arts Collection, courtesy of National Archives of Singapore.
In 1964, the seventh cholera pandemic from nearby Java spread to Singapore. Even though Singapore had been considered vulnerable due to its high volume of traffic as a trading port, the island was able to protect itself from the spread of cholera. By then, its “standards of urban sanitation [were] high, piped water supplies… second to none in Asia, [and] medical control at ports and airports… first class”.36 Several inoculation centres were also set up to offer free vaccines to the population.
Although there are still sporadic instances of cholera infections in sanitised Singapore, with four reported cases as recently as 2009, the virulence of cholera, thankfully, is a thing of the past.37
 Bonny Tan is a former Senior Librarian at the National Library, Singapore. She currently lives in Ho Chi Minh City, Vietnam, with her family and is a regular contributor to BiblioAsia.
Bonny Tan is a former Senior Librarian at the National Library, Singapore. She currently lives in Ho Chi Minh City, Vietnam, with her family and is a regular contributor to BiblioAsia.
NOTES
-
The Free Press. (1841, April 1). The Singapore Free Press and Mercantile Advertiser, p. 3. Retrieved from NewspaperSG. ↩
-
Lee, Y.K. (1978). The medical history of early Singapore (pp. 31, 26). Tokyo: Southeast Asian Medical Information Center. (Call no.: RSING 610.95957 LEE) ↩
-
Untitled. (1851, May 2). The Singapore Free Press and Mercantile Advertiser, p. 5; Untitled. (1851, April 29). The Straits Times, p. 4. Retrieved from NewspaperSG. ↩
-
Hays, J.N. (2005). Epidemics and pandemics: Their impacts on human history (p. 267). California: ABC-CLIO. (eBook) ↩
-
Legislative Council. (1873, October 4). Straits Times Overland Journal, p. 7. Retrieved from NewspaperSG. ↩
-
The year 1895. (1896, January 7). The Singapore Free Press and Mercantile Advertiser, p. 1. Retrieved from NewspaperSG. ↩
-
Snowden, F.M. (2019). Epidemics and society: From the black death to the present (p. 236). New Haven: Yale University Press. (Available for digital loan on nlb.overdrive.com) ↩
-
The Singapore Free Press. (1895, June 27). The Singapore Free Press and Mercantile Advertiser, p. 2. Retrieved from NewspaperSG. ↩
-
A Chinese view – The cholera outbreak. (1895, June 25). The Singapore Free Press and Mercantile Advertiser, p. 3. Retrieved from NewspaperSG. ↩
-
Hallifax, F.J. (1991). Municipal Government. In W. Makepeace, G.E. Brooke & R.St.J. Braddell. (Eds.). One hundred years of Singapore (Vol. I, p. 327). Singapore: Oxford University Press. (Call no.: RSING 959.57 ONE); National Library Board. (2009). MacRitchie Reservoir written by Zaubidah Mohamed. Retrieved from Singapore Infopedia website; Lim T.S. (2018, Apr–Jun). The four taps: The story of Singapore water. BiblioAsia 14, no. 1 (July-September 2018). Retrieved from BiblioAsia website. ↩
-
Correspondence. (1841, April 15). The Singapore Free Press and Mercantile Advertiser, p. 2. Retrieved from NewspaperSG. ↩
-
Cholera. (1873, July 13). The Straits Times Overland Journal, p. 12. Retrieved from NewspaperSG. ↩
-
Correspondence. (1849, October 12). The Singapore Free Press and Mercantile Advertiser, p. 2. Retrieved from NewspaperSG. ↩
-
Local. (1851, January 24). The Singapore Free Press and Mercantile Advertiser, p. 3; The Free Press. (1851, April 25). The Singapore Free Press and Mercantile Advertiser, p. 2. Retrieved from NewspaperSG; Brooke, 1991, p. 505. ↩
-
More about the cholera. (1895, August 12). The Straits Times, p. 3. Retrieved from NewspaperSG. ↩
-
Correspondence. (1873, August 9). Straits Times Overland Journal, p. 11. Retrieved from NewspaperSG. ↩
-
Untitled. (1873, August 9). Straits Times Overland Journal, p. 13. Retrieved from NewspaperSG. ↩
-
Untitled. (1873, August 23). Straits Times Overland Journal, p. 16. Retrieved from NewspaperSG. ↩
-
Legislative Council. (1873, September 20). Straits Times Overland Journal, p. 6. Retrieved from NewspaperSG. ↩
-
Local. (1851, January 31). The Singapore Free Press and Mercantile Advertiser, p. 3. Retrieved from NewspaperSG. ↩
-
Lee, Y. K. (1973, March). Cholera in early Singapore (Part I) (1819–1849). Singapore Medical Journal, 14 (1), 42–48, pp. 44–45. Retrieved from Singapore Medical Journal website. ↩
-
SSR, Z, 33 (65A) 1857, May 1 from Lee, Y.K. (1978). Quarantine in early Singapore (1819–1874) (Part II) (p. 289). Singapore: Stamford College Press (Pte) Ltd. (Call no.: RCLOS 614.46095957 LEE) ↩
-
The “Milton”. (1874, November 19). Straits Times Overland Journal, p. 2. Retrieved from NewspaperSG. ↩
-
Quarantine. (1875, March 6). The Straits Times, p. 1. Retrieved from NewspaperSG. ↩
-
Ng, M., St John’s Island: From gateway to getaway. BiblioAsia 14, no. 1 (April-June 2018). Retrieved from BiblioAsia website. ↩
-
Insanitary Singapore. (1889, December 17). Straits Times Weekly Issue, p. 12. Retrieved from NewspaperSG. ↩
-
Pollution of the Singapore River. (1896, April 28). The Mid-day Herald, p. 2. Retrieved from NewspaperSG. ↩
-
Removal of night soil. (1895, July 15). The Mid-day Herald, p. 2; Municipal Commission. (1895, August 2). The Straits Times, p. 3; Sanitary regulations. (1895, June 24). The Mid-day Herald, p. 2. Retrieved from NewspaperSG. ↩
-
The College of Physicians of Philadelphia. (2020). All timelines overview. Retrieved from The History of Vaccines website. ↩
-
Health in the East. (1928, January 11). The Straits Times, p. 9. Retrieved from NewspaperSG. ↩
-
New move to prevent cholera spread. (1937, August 21). The Singapore Free Press and Mercantile Advertiser, p. 1. Retrieved from NewspaperSG. ↩
-
Cholera menace. (1961, September 7). The Straits Times, p. 8. Retrieved from NewspaperSG. ↩
-
National Centre for Infectious Diseases. (2020). Cholera. Retrieved from National Centre for Infectious Diseases website. ↩

